We must stop squandering our precious antibiotics

"One solution is to increase the supply of new drugs." Image: REUTERS/Brian Snyder

Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:
Davos Agenda
Like so many breakthroughs, it happened almost by accident. In the late 1940s, fishermen near Lederle Laboratories, in New York state, noticed that the trout they were catching were getting bigger. Word reached a biochemist called Thomas Jukes, who thought it might have something to do with the run-off from Lederle’s latest miracle product - an antibiotic called aureomycin.
So he and his colleague Robert Stokstad tried an experiment. They took some newborn chicks, and fed one group on a liver extract, designed to cure anaemia. Another was given aureomycin.
The results were startling: the birds given the antibiotic didn’t just survive, but put on weight with extraordinary rapidity. When this discovery was officially announced in 1950, the New York Times proclaimed that aureomycin’s “hitherto unsuspected nutritional powers” would have “enormous long-range significance for the survival of the human race”.
In the 65 years since, antibiotics have cured millions of people of infectious diseases, as well as filling billions of stomachs by helping chickens, pigs and cattle get ever larger. But their use in gargantuan quantities, with poor controls, has left us facing a new threat: drug-resistant bacteria.
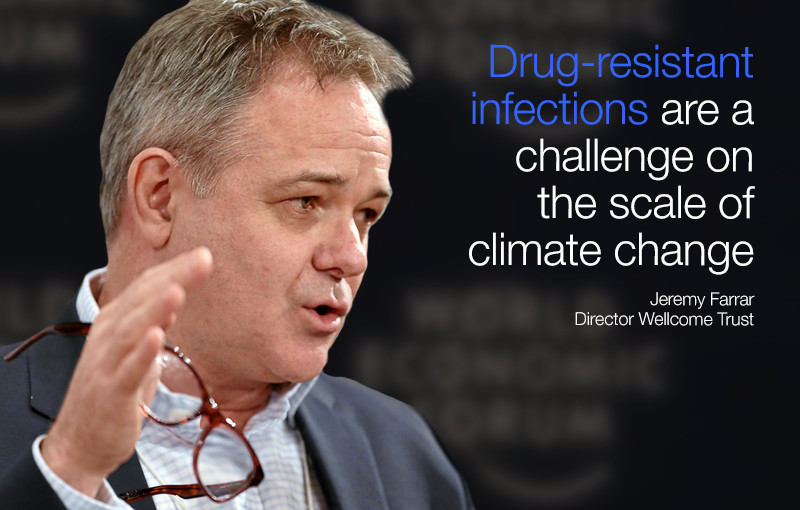
The independent Review on Antimicrobial Resistance, backed by the UK government and the Wellcome Trust and headed by the economist Jim O’Neill, estimates that by 2050, infections that are untreatable with antibiotics could cost the global economy $100 trillion and kill 10 million people a year. And when it comes to fighting them, our cupboard is almost bare: we have developed no new classes of antibiotics for 25 years. This is a problem that rivals climate change.
One solution is to increase the supply of new drugs. We have failed here not for want of ingenuity, but for want of incentives. It is difficult, often even impossible, for any antibiotic to make money in the current system. These are low-priced drugs taken for short periods of time, but use at the volumes needed to turn a profit is exactly what builds resistance. The O’Neill review has recommended new funding mechanisms to stimulate antibiotic development that I hope will be taken forward in Davos this week. But we must tackle demand as well as supply.
Some 70 per cent of medically important antibiotics in the US are given not to people but to animals. The global proportion used in agriculture is hard to calculate, but the O’Neill review estimates it is at least half. As evidence mounts of a link between agricultural antibiotic use and resistant infections in people, it is clear that we are taking unacceptable risks. Antibiotic use for growth promotion should be banned: there are acceptable alternatives, as a ban in Denmark has shown. Where antibiotics are needed to treat sick animals, these should be restricted to classes that have no human medical use.
Go on as we are, and we will jeopardise more critical drugs like Colistin, a last-resort treatment against bacteria that have become resistant against other antibiotics. Colistin is used widely in agriculture, and in November, it was revealed that E. coli bacteria in China, in both pigs and people, have acquired resistance to it. The same gene has now been found in E. coli in Europe. We are recklessly losing something we should have taken great care to protect.
As we tackle agricultural misuse of antibiotics, we must also take on overuse in human medicine. One key to that is better public engagement. Last year, Wellcome carried out a wide-ranging study of UK public attitudes to antibiotics. It showed that people see them almost as magic pills: a prescription, whatever your actual illness, is evidence that you’re really suffering. So powerful is this effect, according to research from King’s College London, that doctors who limit antibiotic prescriptions receive worse ratings from patients.
This is fed by a lack of awareness of antibiotic resistance. Our research revealed that many people simply don’t understand what those words mean. Most interpret it as their own bodies becoming resistant to the drugs, which is one reason they stop taking them too early -- a major contributing factor to the development of resistance.
It’s the same when we talk about the scale of the problem. I warned above that drug-resistant infections could cost us millions of lives and trillions of dollars, that it is a challenge comparable to climate change. Such phrases may get heads nodding at Davos, but they are mostly ignored by the general public. When we use such grand language, our research showed, people assume that we’re exaggerating, or that scientists will fix things, or that the problem lies far in the future.
We need to communicate better. Rather than talking about “antibiotic resistance”, we should say “drug-resistant infections”: we found that putting the focus on the bacteria, not the patient, improves understanding. We should also illustrate the problem through specific, familiar and contemporary threats: the idea that E.coli, tuberculosis or salmonella will become harder to treat, or that Caesareans, chemotherapy or hip replacements will become difficult to conduct.
The WHO considers drug-resistant infection to be the greatest challenge in infectious disease. It is already killing hundreds of thousands of people in developed and developing nations. But we know what needs to be done: increase the supply of new antibiotics, and cut the demand for existing ones, by restricting their use in agriculture and doing a better job of explaining the problem.
Thomas Jukes believed that antibiotics were an astonishing force for good. He was right, even if their “nutritional powers” have proved double-edged. We must value these remarkable drugs, and deploy them with due care and attention, if we are not to squander their continuing potential to save and improve lives.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
The Agenda Weekly
A weekly update of the most important issues driving the global agenda
You can unsubscribe at any time using the link in our emails. For more details, review our privacy policy.
More on Davos AgendaSee all
Kate Whiting
April 17, 2024
Andrea Willige
March 27, 2024
Shyam Bishen
March 20, 2024
Simon Torkington
March 15, 2024
Miranda Barker
March 7, 2024