The weight of inaction: why is the impact of obesity not being taken seriously?

Obesity is misunderstood, with blame placed on the individual for personal lifestyle failure. Image: Shutterstock / DisobeyArt
- Obesity is a chronic, progressive and relapsing disease that impacts 650 million people worldwide.
- People living with obesity face reduced quality of life, increased risk of cancer and premature death.
- Obesity impacts national economies with increased healthcare costs and a reduction in workforce productivity.
Obesity is a serious, chronic, progressive disease that kills at least 4 million people per year. People living with obesity have an increased risk of developing other health conditions, such as heart disease, type 2 diabetes and certain types of cancer.
Beyond the significant impact on people living with obesity, the collective impact on public health puts significant strain on healthcare systems around the world. Reports suggest treating obesity-related issues accounts for an average of 8.4% of total healthcare spending in Organization for Economic Co-operation and Development (OECD) countries. Obesity also impacts employment; research, by the OECD, suggests its impact equates to a reduction in the workforce of 54 million people per year across the 52 countries analysed, reducing GDP by 3.3%.
Despite its obvious global impact, obesity is misunderstood, with blame placed on the individual for personal lifestyle failure. The reality is many of those living with obesity remain underdiagnosed, under-supported and under-treated, which can make achieving sustainable weight loss, or even asking for help in the first place, impossible.
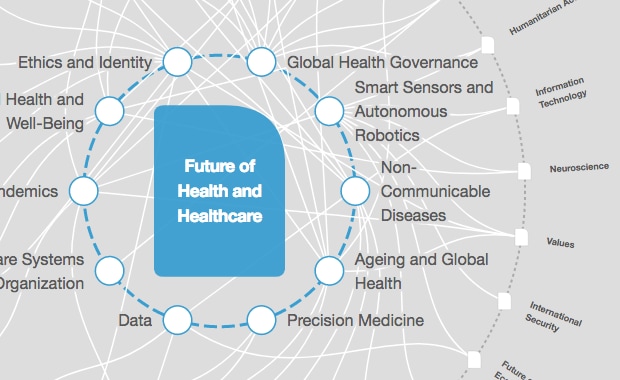
How is the World Economic Forum bringing data-driven healthcare to life?
Barriers rooted in stigma and bias against obesity
Weight stigma is as prevalent as discrimination on the grounds of age and race and is recognized for its detrimental impact on obesity outcomes. Pursuing weight loss is challenging and the culture of shame around obesity can prevent people from attempting to access needed advice, from personal and professional channels.
This stigma is compounded by the language surrounding obesity, which suggests individual choices are to blame in a way that other diseases do not suffer from. The reductionism of treating obesity as a result of poor lifestyle choices ignores the critical role of genetics and socio-economic influences.
In addition, attitudes to obesity can vary culturally. Research shows that black and Asian children are three times more likely to be obese than white children. In some cultures, being overweight is a societal signal of wealth and good health and, combined with cultural food practices, can place a greater emphasis on consuming greater volumes of high-fat foods.
Studies also show that stigma creates unfavourable policies that prevent access to care, based on beliefs that people living with obesity are less deserving of comprehensive care and treatment. This has led to a lack of policy prioritization and legislation, such as in Germany and Italy, where reimbursement for weight regulation is forbidden by law.
To address this, in March 2022, the European Parliament Interest Group on Obesity and Health System Resilience published a joint declaration to encourage countries to apply a non-communicable disease (NCD) framework for obesity as a chronic disease. To ensure obesity achieves parity with other diseases, this called for better treatment pathway guidelines, funding instruments and specific education and training for healthcare professionals.
Initiatives like this create the momentum needed for action, but policy shifts have not been implemented at scale and have not been adequately informed by relevant, cultural nuances. Today, no member state in the WHO European Region is on track to reach the Sustainable Development Goal target of halting the rise in obesity by 2025, affecting almost 60% of adults in the region.
What will make a difference?
Priority actions to tackle obesity must be focused on prevention and treatment. We’ve learned from other disease areas that preventative measures are essential and public awareness campaigns, regulation and taxation on products promoting unhealthy habits can improve population health — see the success of stop-smoking campaigns in lung cancer. Prevention is a long-term strategy, however. It cannot help people who are already living with obesity, where urgent action is needed now to support access to treatment.
National and local public health initiatives can drive change through culturally relevant programmes that equip individuals with the tools they need to help them manage their weight, in the context of their cultural and religious norms.
Without action, the average economic cost is projected to reach more than 3% of GDP in 2060, with the biggest increases expected in lower-resource countries. If overweight and obesity prevalence is reduced by 5% between 2020 and 2060, the potential total savings could be $429 billion per year on average.
The world cannot afford not to act on obesity. Change is critical to economic resilience, but addressing obesity cannot be left up to individuals to manage alone, without concerted and holistic action in obesity care. Collaboration between governments, industry, healthcare professionals and non-governmental organisations (NGOs) is critical to delivering better healthcare outcomes for those living with obesity today and to preventing future generations suffering from this disease.
We can build on the experiences of addressing other public health issues and chronic diseases, to change the way we view and care for people living with obesity. To do so, we must prioritize policies that prevent and treat obesity, tackle stigma and reduce the emotional barriers for people to seek help.
Healthcare systems that make obesity care accessible, without judgement, and encourage positive health-seeking behaviours can help create a healthier and more sustainable future than the one we face today.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
Health and Healthcare
Related topics:
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Mansoor Al Mansoori and Noura Al Ghaithi
November 14, 2025