These are the 5 primary factors that indicate a successful vaccine rollout

Some places have better access to vaccines than others. Image: REUTERS/Nick Lachance
- Access to and uptake of COVID-19 vaccines has been heterogeneous and uneven, with more advanced economies having a larger share of vaccinations.
- Vaccines appear to retain efficacy against the highly infectious Delta variant but have a lower marginal impact compared to other strains.
- However, the mutation of the virus suggests that no country is safe, write experts.
- Results suggest that new COVID-19 cases in neighboring countries contribute to an increase in a country’s own infections.
Vaccination is understood to be the way out of the COVID-19 pandemic and the economic crisis it engendered (Gopinath 2020). However, access to and uptake of COVID-19 vaccines, especially in the early phase, has been heterogeneous and uneven. Countries in North America and Europe started vaccinations earlier and are further along than regions such as Africa and the Middle East. Across income groups, advanced economies have vaccinated a much larger share of their populations than emerging and developing economies, on average.
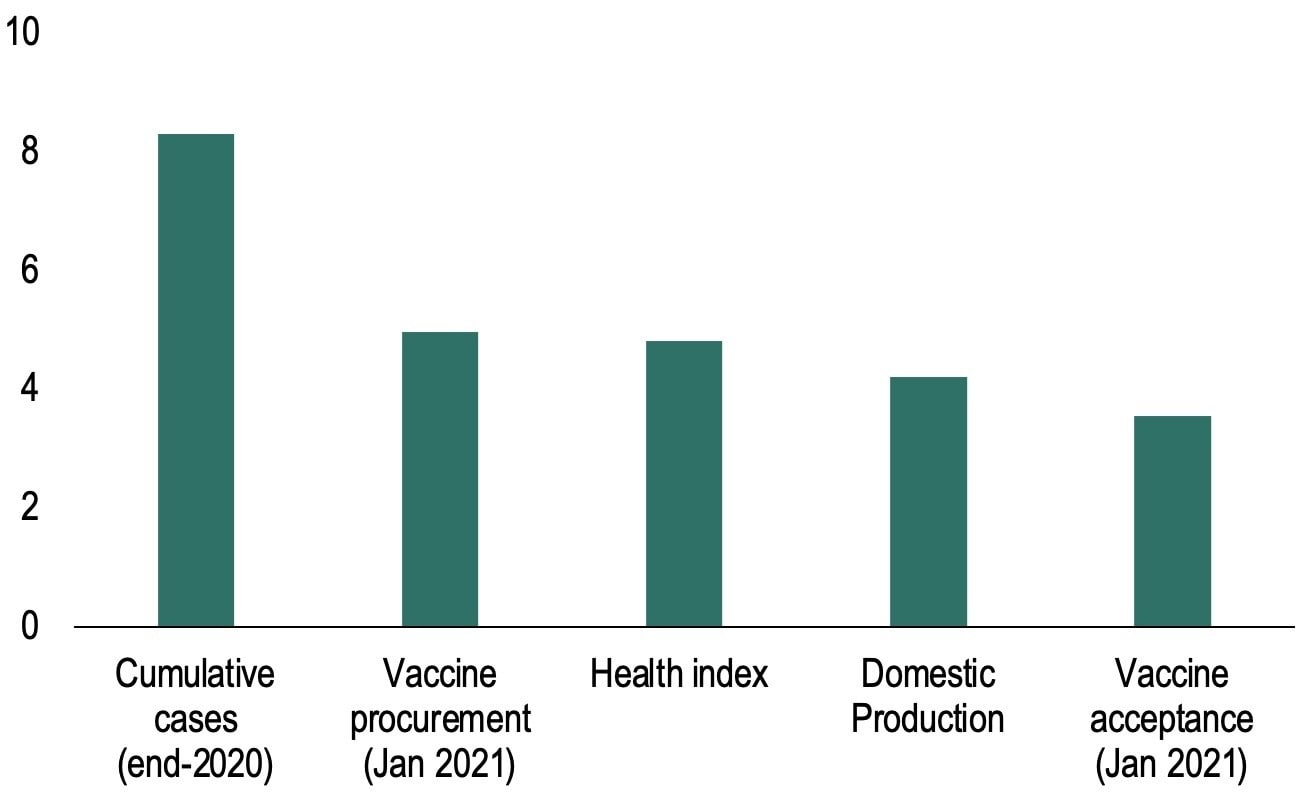
Our empirical analysis (Deb et al. 2021a) uses cross-sectional variation in vaccination rates (as of July 2021) to ascertain which demand and supply factors explain these cross-country differences in vaccine rollouts. Our results suggest that the severity of the COVID-19 waves in 2020 was the leading driver (Figure 1): countries more affected in terms of cases (for example, the US) had higher vaccination rates in the first half of 2021, potentially reflecting greater urgency to vaccinate. A population’s willingness to receive the vaccine also made a difference (Figueiredo et. al. 2020, Dewatripont 2021).
Supply-side factors such as early procurement played a critical role in explaining the pace of rollouts. The difference in procured vaccines (confirmed and potential deals) in January 2021 between countries which acted early (e.g. Israel) and those where negotiations were protracted (e.g. Germany) is associated with a four percentage-point difference in vaccination rates. Domestic production of vaccines also matters and is associated with higher and faster vaccination rates. This reflects the ability of producing countries like China to secure a larger vaccine supply and administer them more quickly. Finally, health infrastructure – hospitals, medical facilities, and doctors per capita – also contributed.
Figure 1 Determinants of vaccine rollouts
Factors affecting vaccine rollouts (impact of one standard deviation change in factor on vaccinations per 100 population)
Vaccinations to end the health crisis
Our analysis quantifies the effects of vaccines per capita on health outcomes using real-time data for a large sample of countries. Daily data on the number of new COVID-19 infections, fatalities, and intensive care unit (ICU) admissions are used along with data on containment policies, state of the pandemic, and the dominant variant of the virus.
The results suggest that COVID-19 vaccines have been effective in reducing infections, fatalities, and ICU admissions, consistent with epidemiological studies (Dagan et. al. 2021, Hall et. al. 2021 among others). A ten percentage-point increase in the administration of the first vaccine dose per capita (similar to the rollout in Singapore between February and early March 2021) is associated with a reduction in daily new cases by –0.01 percentage points of the population (about half a standard deviation) after 21 days, and a decline in the reproduction rate (the number of secondary cases that would be generated by an index patient) by –0.14 percentage points (Figure 2). In addition, vaccination reduces the number of COVID-19-related ICU patients and fatalities, helping to ease strains on health infrastructure.
The health effects of vaccines increase after their administration, in line with the epidemiological literature, and the second dose contributes to further flattening the pandemic curve by reducing the virus reproduction rate. There is also evidence that the effectiveness of vaccines varies depending on the dominant COVID-19 variant: vaccines appear to retain efficacy against the highly infectious Delta variant but have a lower marginal impact compared to other strains.
What is the World Economic Forum doing about access to vaccines?
Figure 2 Effect of COVID-19 vaccines on health outcomes
(percent of the population, share of COVID-19 cases)

Vaccine spillovers
The mutation of the virus into more transmissible strains suggests that no country is safe, even those achieving high vaccination outcomes. Indeed, the rapid spread of the Delta variant from India to neighbouring countries highlights the cross-border risks from protracted waves – for instance, the Delta variant became the dominant coronavirus in ASEAN countries and in North America over a one- to three-month period after becoming the dominant variant in India (Figure 3, top panel).
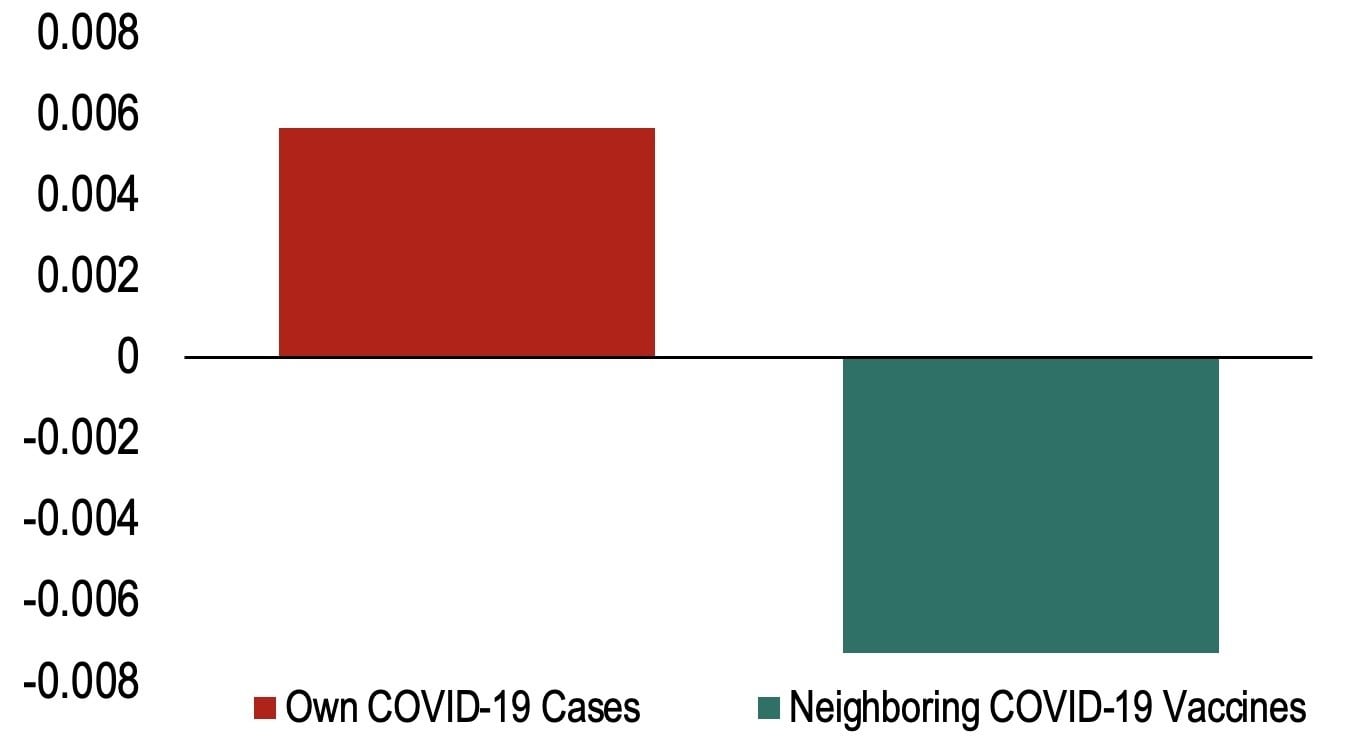
To shed light on spillovers, our empirical analysis constructs daily proxies of ‘foreign’ COVID-19 cases and vaccines in neighbouring countries, based on geographic proximity and trade linkages. The results suggest that new COVID-19 cases in neighbouring countries contribute to an increase in a country’s own infections (Figure 3, bottom panel), as movement across borders increases transmission. On the other side of the coin, there are favourable spillovers from increased vaccinations in neighbouring countries. These spillovers provide compelling evidence for international cooperation to ramp up vaccine production and ensure adequate distribution to all countries, including by sharing excess doses (Lamy 2020).
Figure 3 Spillovers from COVID-19 outbreaks
a) Days elapsed until Delta variant reached 50% of COVID-19 cases (number of days)
b) Effect of neighbouring COVID-19 cases and vaccines on a country’s health outcomes (percent of population)
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
Vaccination
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Mansoor Al Mansoori and Noura Al Ghaithi
November 14, 2025








