Financing heart failure care in Asia Pacific: The case for investing now

Heart failure affects nearly 32 million people in the Asia Pacific. Image: Unsplash/Quan-You Zhang
- Heart failure affects nearly 32 million people in the Asia Pacific, costing health systems more than diabetes, despite affecting far fewer people.
- Smart investments in early detection, registries and community-based care can reduce hospitalization, lower costs and improve long-term outcomes.
- Sustainable financing – from reallocating budgets to innovative models such as sin taxes – can bring heart failure out of the policy shadows.
Nearly 32 million people in Asia Pacific are living with heart failure – a condition that consumes more health spending than diabetes despite affecting far fewer people. Yet, it remains largely invisible in policy discussions, even as it quietly pushes health systems towards unsustainable costs.
Heart failure is not an isolated issue: it is the severe end of the region’s broader cardiovascular disease crisis, which is already the leading cause of death. But heart failure stands out from many other non-communicable diseases, with 6 million admissions annually across the region.
Once advanced, heart failure is far more difficult to reverse, making early investment essential and fiscally prudent.
The cost of inaction
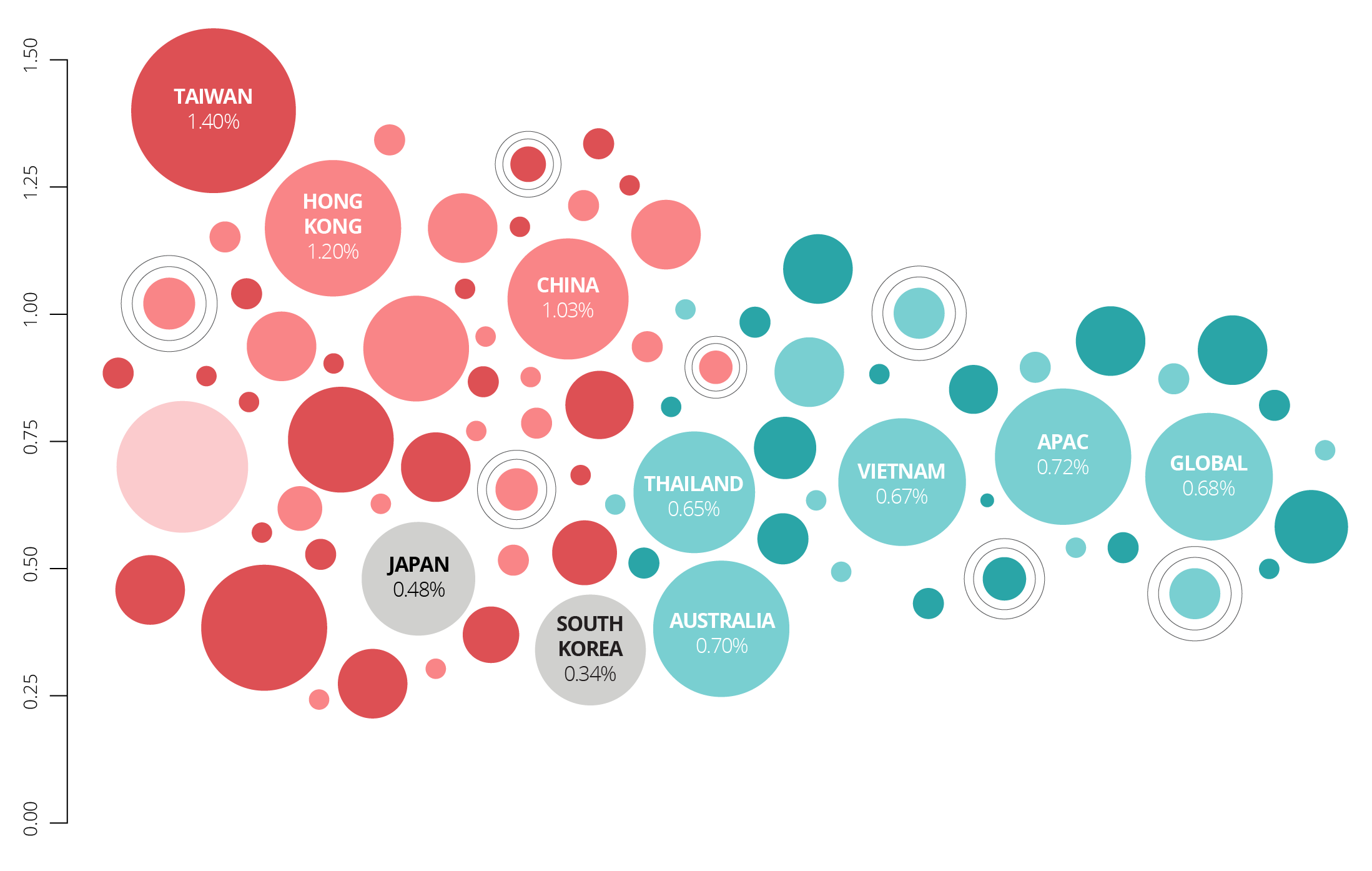
In Asia Pacific, heart failure accounts for an estimated 8-10% of national health expenditure for the 32 million patients living with the condition. In contrast, diabetes, which affects 200 million people, more than six times the number of people with heart failure, accounts for only about 5% of health expenditure.
This imbalance reflects a reactive model of care and one that waits until patients reach an acute crisis. Late detection, heavy reliance on hospitalization and fragmented long-term care drive significant and unavoidable costs for governments.
With rapidly ageing populations and the rise of non-communicable diseases, health systems in the region are approaching a fiscal tipping point. Progress towards the UN’s Sustainable Development Goal of reducing premature non-communicable disease deaths by a third by 2030 has stalled.
Political commitment toward heart failure and cardiovascular diseases specifically remains low, often lost within the broader non-communicable disease agenda, with few measurable targets or dedicated funding. Considering that heart failure is typically a consequence or co-morbidity of other non-communicable diseases, the Asia Pacific region faces a grave challenge.
As many governments prepare their 2026 budgets, the case for earmarking funds for smarter heart failure management is compelling. Delaying action will only drive up costs and worsen outcomes. Proactive investment today will lower healthcare costs tomorrow.
Prevention across the continuum of care
Beyond its clinical toll, heart failure severely affects quality of life, fuels depression and anxiety, and is a heavy burden on caregivers who often lack support.
Its impact ripples across families, workforces and national economies. In fact, the Asian Development Bank has warned that non-communicable diseases already are a barrier to economic growth – and heart failure exemplifies this concern.
Yet, the evidence shows that when prevention and management are strengthened across the heart failure continuum – from early detection to long-term follow-up – hospitalizations reduce and outcomes improve. Take, for example, Hong Kong, where heart failure is one of the costliest complications of type 2 diabetes, adding almost $13,000 annually per patient.
A study of its public health system found that introducing the biomarker test NT-proBNP to screen and proactively treat high-risk patients reduced costs by approximately $850 per patient, while extending life by approximately 0.13 years. Early investment clearly pays off.
3 smart investments to transform heart failure care
Although national healthcare budgets are indeed finite, practical and sustainable solutions exist to fund proactive and preventive care. Governments and policymakers should focus on high-impact interventions across the heart failure pathway:
- Primary care – reimbursement of screening tools: Making biomarker testing available and reimbursable at the point of care, especially in community clinics, enables faster and more equitable diagnosis. An earlier diagnosis means treatment can begin sooner, thus delaying or preventing the onset of heart failure.
- System level – building in data gathering and registries: Investing in national heart failure registries linked to regional collaboration, will standardize data, improve monitoring and allow countries to learn from one another. Smarter data means smarter financing, better policy design and more efficient resource allocation.
- Tertiary care – long-term care strengthening: Follow-up care and rehabilitation are critical yet often not prioritized. Expanding follow-up via multidisciplinary heart failure clinics, digital health tools and community-based workforce models will enhance long-term patient outcomes and build more resilient chronic care systems.
Together, these reforms create a clear and actionable roadmap for countries at different stages of health system maturity.
They also reinforce the outcomes of the recent UN General Assembly high-level meeting on non-communicable diseases and mental health, which called for integrating non-communicable disease services into primary care as the foundation of universal health coverage and supported by sustainable, resilient health systems that enable health promotion, prevention, screening, diagnosis, treatment and rehabilitation.
Decisive action today to safeguard tomorrow’s future
By investing in early detection, stronger systems and community-based care, the Asia Pacific region can build a clear, actionable roadmap to improve heart failure outcomes across diverse health system contexts, while ensuring fiscal sustainability.
For lower- and middle-income countries, competing health priorities mean heart failure care risks being deprioritized. This makes innovative financing models essential – from reallocating budgets towards preventive health, to “sin taxes” or integrating services for related diseases.
As the Asian Development Bank highlights, such measures can stretch limited resources further while ensuring sustainable coverage. By funding prevention at every stage – including screening, diagnosis and long-term care – the Asia Pacific can reduce the burden of heart failure, improve patient outcomes and ease the long-term strain on healthcare systems and societies.
Heart failure is silently claiming lives across the Asia Pacific but it does not have to remain hidden in the policy shadows. The time for fragmented approaches is over.
Governments must act now to prioritize heart failure prevention and care or risk shouldering even greater costs in the future. Decisive action today will not just save millions of lives but also safeguard the region’s economic future.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
SDG 03: Good Health and Well-Being
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Priya Abani
February 18, 2026






