Pivoting health research to take on COVID-19 - What one team learned

Colorized scanning electron micrograph of apoptotic cell infected with novel coronavirus Image: via REUTERS
Steven R. Steinhubl
Director of Digital Medicine, Scripps Research Translational Institute, Staff Cardiologist, Alaska Native Tribal Health ConsortiumAn urgent weekend email from an old friend set everything in motion. He was worried about the gathering storm of COVID-19, and had woken up at 5:30 in the morning with a racing mind - and a simple question: Could we pivot our longstanding health research program to take on the rapidly growing pandemic?
Over the last few years, Scripps Research has been a pioneer in exploring how wearable devices like activity trackers and smartwatches can provide valuable health insights, including a more precise identification of viral infections. Our friend wondered whether we could use that expertise to spot COVID-19 outbreaks long before people start showing up at doctors’ offices or emergency rooms.
In the two weeks since we received that email, we’ve been working around the clock—and racing against time - to organize a study that, under ordinary circumstances, might have taken months or even years to come together.
What is the World Economic Forum doing about the coronavirus outbreak?
Leveraging prior research
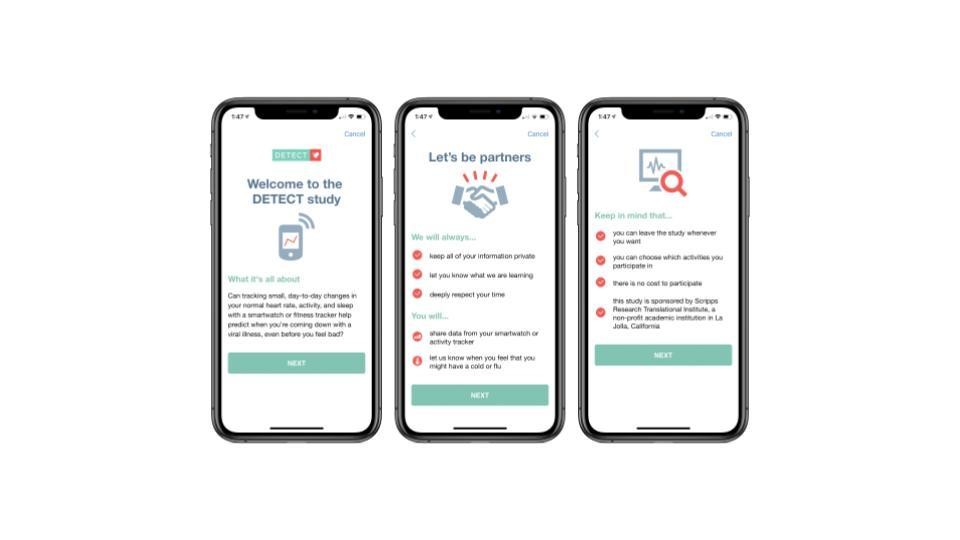
The DETECT health study, which we’ve just launched, will “crowdsource” heart rate data from a large number of volunteers who have wearable devices (keeping all data in the strictest confidence and ensuring it's stripped of any personally identifying details before analysis). The study will explore whether subtle changes in an individual’s heart rate could help identify viral illnesses like COVID-19 before people are aware of any symptoms.
DETECT builds on recently published work from our digital medicine group, including one study that analyzed two years of heart rate and sleep data from 47,249 Fitbit users and discovered a very high correlation (around 0.9) between Fitbit data and CDC reports about flu outbreaks. That means wearables might help us predict the prevalence of flu in a community.
"Now is the time to explore innovative approaches"
”Another study analyzed two years of resting heart rate data from 92,457 Fitbit users in the U.S. It found that resting heart rates vary widely in the population, but they are surprisingly stable on an individual level, and temporarily increase when we get sick.
Of course, the DETECT study has just begun, and there's no proven connection yet between wearables data and COVID-19. We're hoping, though, that our research might someday provide an early warning to both individuals and public health officials.
As we write this, COVID-19 remains a grave threat to human health worldwide. Deficiencies in our surveillance methods have allowed the novel coronavirus to spread silently in numerous countries. The resulting explosion of exponential growth at the community level has already overwhelmed the health care system in Italy, and is poised to do so elsewhere as well. Now is the time to explore innovative approaches like DETECT for identifying and containing viral outbreaks.
Lessons learned
In our rapid development of DETECT, we’ve learned that quickly pivoting a research program can be challenging. People and institutions tend to have a certain inertia, and it’s not easy to alter their speed or course. Working within a compressed timeline, we’ve had to make changes and accommodations in order to reach ambitious goals. Here are some of the lessons we've learned:
- Pause existing projects. In our experience, it’s crucial, if possible, to pause existing projects. This is not the time to be multitasking. Focus all of your efforts on COVID-19. With lives hanging in the balance, other work can wait.
- Expect fluid, flexible roles. We’ve found that creating more fluid and flexible roles for team members has been crucial to achieving success. In traditional projects, each person typically has a narrowly defined scope of responsibilities. That’s fine when working according to existing templates in a familiar domain. But it’s a recipe for disaster in this fast-moving, sometimes chaotic environment. Instead, adopt the agile mindset of a start-up, in which each person wears many hats, pitching in as needed.
- Start key conversations early. Researchers rarely have complete autonomy, so it’s important to reach out as early as possible to those on whom you depend. For example, soon after the DETECT study took shape, we connected with the chair of our institutional review board, asked many questions, and arranged an expedited process for evaluating our paperwork for human subjects research. We also worked closely with an existing software development partner to ascertain whether our plans and timelines were technically feasible.
- Consider new ways of working. “Thinking outside the box” has become a hoary cliché, but under current circumstances, it’s actually essential advice. Time and again over the last two weeks, we’ve run into roadblocks and even the occasional dead end. Had we been content to do things only as we’d done them in the past, it’s unlikely that the DETECT study would now be live. Instead, we’ve been forced to invent new ways of operating, often requiring far fewer resources and far less time. The website that we built for the study is a case in point. Instead of an entirely custom design, we leveraged previous work so that the website could be launched quickly.
We must marshal all available resources—including biomedical research capabilities—in our battle against COVID-19. It’s been heartening to see research groups around the globe stepping into the breach, often pivoting radically from their ongoing work. We hope that many more will choose to do so. Together, we can develop the tools and the knowledge that will support those who are fighting on the front lines.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
Global Health
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Mansoor Al Mansoori and Noura Al Ghaithi
November 14, 2025







