Stop playing catch-up with superbugs: the anticipatory governance of antimicrobial resistance
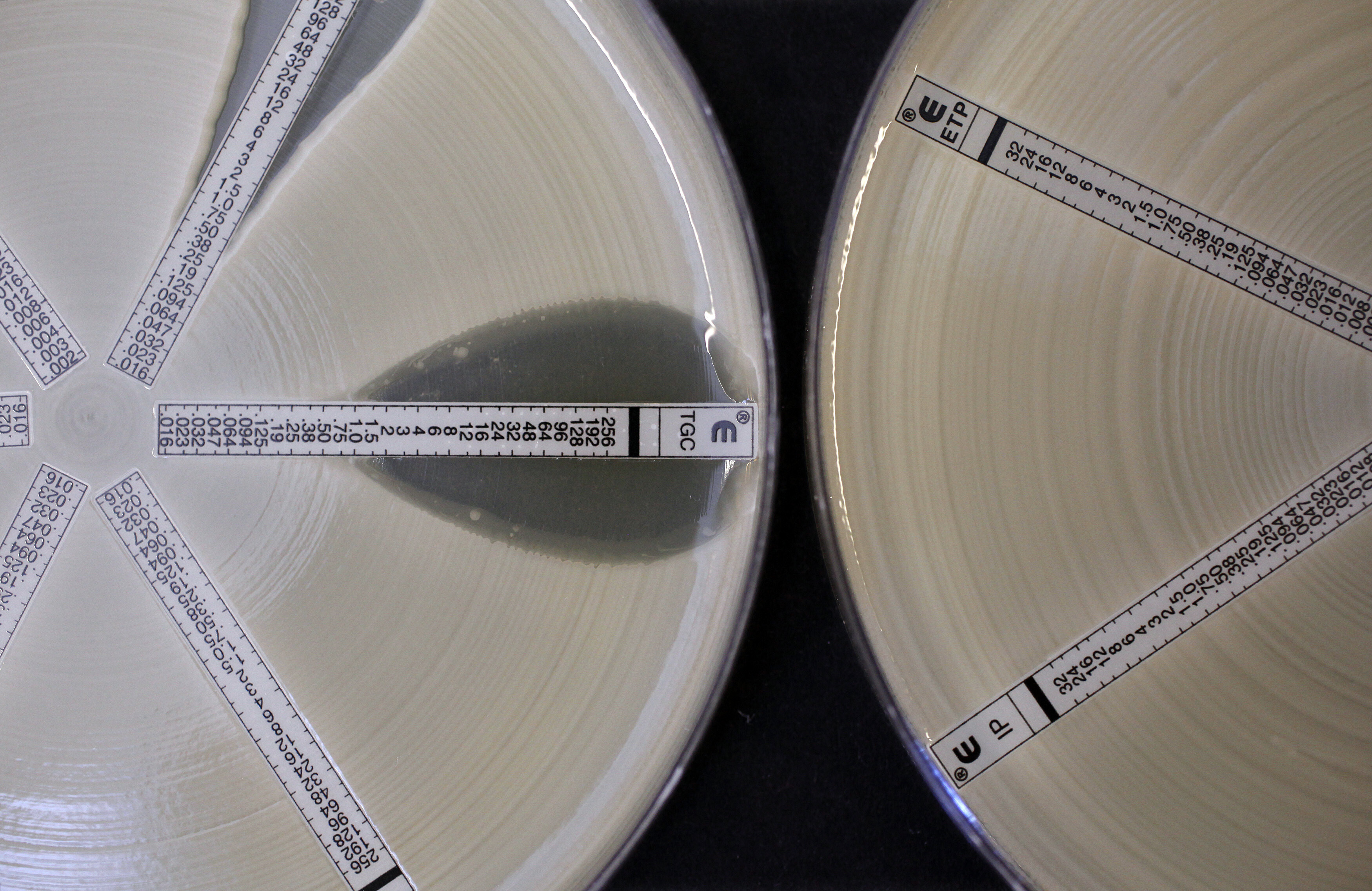
Fast-rising antimicrobial resistance (AMR) threatens lives, global healthcare systems and the world economy. Image: Reuters/Suzanne Plunkett
- Fast-rising antimicrobial resistance (AMR) threatens lives, global healthcare systems and the world economy.
- Anticipatory governance can enhance AMR surveillance to project multiple possible outcomes and identify the best intervention points.
- It can also coordinate siloed healthcare operations into a comprehensive, multisectoral system.
Over billions of years, bacteria have built a vast resistome; a genetic archive that equips them to face challenges we are only beginning to understand. Endlessly inventive and highly responsive, they swap genes, produce chemical defences and thrive in every environment, from oceans to caves to tundra.
By the time humans arrived, bacteria had already shaped infectious disease threats that followed us through history. The discovery of penicillin and the ensuing “golden antibiotic era” allowed us to stand on equal footing with bacteria. But within a century, their relentless adaptability has undermined the effectiveness of our available antibiotics. This problem, antimicrobial resistance (AMR), contributes to more than 4.5 million deaths every year at unfathomable economic cost.
Despite this fast-growing threat, our global response remains dangerously slow. At a high-level meeting in 2024, the UN made promising commitments, yet solutions to this existential threat remain vastly under-prioritized and under-resourced. If this continues, the centre will not hold. Already, we are at risk of:
- A declining R&D workforce and the collapse of the antimicrobial pipeline.
- Accelerating resistance rates and projected cost to the global economy in the trillions.
- As much as 10% of the value of the world’s publicly traded companies exposed to AMR-related risks.
- Routine healthcare events like childbirth, cancer care and surgery carrying ever-increasing infectious risks.
The warning signs are everywhere, and it is imperative that we heed the call. One way to close the gap between warning and response is through anticipatory governance, acting early and staying ahead of the threat.
Anticipatory governance emphasizes foresight, inclusiveness and adaptive policy to address risks before they escalate to insurmountable crises. Rather than reacting to events after they unfold, it involves building institutional capacity to detect weak signals, assess future scenarios and act decisively on early warnings. The approach has been applied in diverse domains, from climate to emerging technologies and conflict resolution.
From forecasting to future-casting
Surveillance, the systematic tracking of microbial threats, is central to AMR control, yet current systems are slow, fragmented and inconsistent. These gaps create blind spots, particularly in low- and middle-income countries, where infrastructural and diagnostic inconsistencies slow responses. By rethinking how we collect and use surveillance data, anticipatory governance can transform surveillance into early-warning systems.
Surveillance must shift from forecasts to foresight, exploring multiple possible futures rather than predicting the most likely one. Foresight continuously interprets emerging signals to reveal hidden risks, while challenging assumptions that may limit effective action. This dynamic process of sense-making and sense-breaking transforms surveillance into a proactive tool for anticipating threats, stress-testing scenarios and guiding early interventions. It leverages AI, predictive models, trend analysis and scenario simulations to map antibiotic-resistance trajectories and identify the most effective points for intervention.
Some programmes are already pushing AMR surveillance into the future. The EU’s EpiPulse platform tracks pathogens and resistance genes across member states, giving countries a clearer view of cross-border AMR trends. The UK’s Oxford Nanopore partnership brings real-time genomic sequencing into NHS hospitals to identify resistant pathogens within hours. Globally, rapid clinical sequencing of drug-resistant bacteria is emerging, complemented by wastewater monitoring, showing how surveillance can move from passive reporting to actively anticipating and responding to AMR threats.
By integrating real-time data from clinical, social, digital and environmental sources, as well as genomic sequencing and supply chain data, health authorities can guide allocate antimicrobial resources strategically, implement targeted interventions and inform R&D priorities.
From silos to systems
AMR impacts health, but tackling it could reshape healthcare and beyond. Fragmented governance architectures, siloed operations and limited capacity currently prevent a holistic response, with many stakeholders perceiving AMR solely as an infectious disease problem. Hospitals, laboratories, academics, implementers and policy-makers each hold partial insights, but weak interconnections hinder coordinated action.
Anticipatory governance fosters collaboration through inclusive, participatory mechanisms that engage a broader range of actors, including all government ministries and departments, as well as private sector and civil society. These mechanisms harness the sense-making and sense-breaking strategies enabled by foresight, challenging entrenched assumptions and siloed practices while fostering transparency, legitimacy and a mandate to act across sectors.
Promising approaches illustrate the potential of this inclusive model. In the UK, the NHS antimicrobial subscription model explores new ways to align incentives for drug development, incorporating input from clinicians, regulators and patient groups to guide prioritization and use. Drawing from examples such as the US Armed Forces Antimicrobial Monitoring and Research Programme, African military medical services are also exploring partnerships with national authorities and local communities to extend surveillance into hard-to-reach areas; they use World Health Organization recommendations on structured civilian-military collaboration for health emergencies.
Across these approaches, multisectoral working groups and shared platforms allow diverse actors to interpret emerging trends, question assumptions and explore coordinated strategies before crises escalate. Broad engagement, transparent decision-making and shared capacity and authority lay the foundation for a resilient, integrated approach to AMR.
From reaction to resilience
Bacteria will always evolve, no matter what strategies and medicines we develop. Anticipatory governance provides an optimal lens through which to view this challenge because it embeds adaptive policy into routine practice, so early warnings trigger decisive action rather than being lost amid shifting priorities. Mainstreaming surveillance, decision-making and capacity-building enables governments to act in real time, while maintaining long-term strategies.
A core element of adaptive policy is linking surveillance insights to actionable thresholds. Governments can define indicators that trigger interventions, from intensified stewardship and revised treatment guidelines to targeted infection control and strategic investments in R&D, diagnostics and infrastructure. In Sweden, for instance, the government has invested in structured national monitoring of antibiotic use and resistance trends, as well as clinical research, to support regular update of treatment guidelines.
Adaptive policy also supports experimental and anticipatory approaches, such as pilot programmes, data-sharing platforms and multisectoral working groups. This allows stakeholders to interpret signals, test assumptions, and define and refine strategies collaboratively. By embedding thresholds, triggers and iterative learning, governments can create a resilient policy ecosystem focused on long-term outcomes. Flexible, evidence-based and participatory interventions ensure that AMR policy remains resilient to an evolving threat landscape.
How the Forum helps leaders strengthen health systems through collaboration
The threat of antimicrobial resistance is evolving in a crowded global health landscape filled with urgent challenges, where health systems and societies are often forced into constant reaction rather than anticipation. Anticipatory governance offers a way to break this cycle: Through foresight, inclusiveness and adaptive policy, we can contain resistance more effectively, proactively shaping mitigation strategies across sectors and leveraging new technologies. By investing in these approaches now, we strengthen our capacity to act purposefully.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
Global Health
Related topics:
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Priya Abani
February 18, 2026






