How to make healthcare sustainable and equitable for a better future

The healthcare sector can drive better outcomes with fewer resources through the use of digital, AI-enabled and sustainable solutions. Image: Rology
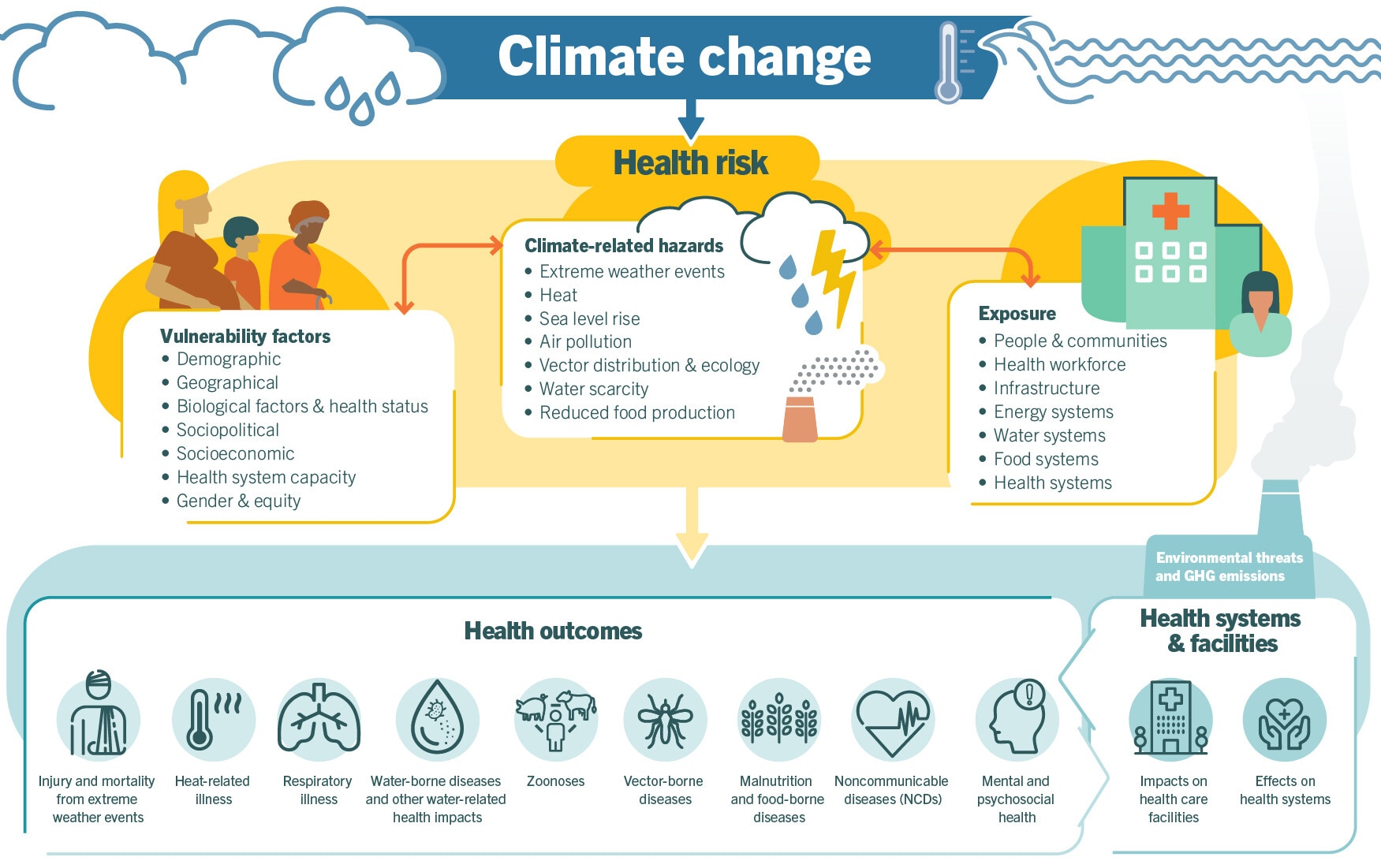
- As global conflict and environmental disasters exacerbate equitable healthcare challenges, the sector is well placed to drive responsible and sustainable practices.
- Reimagining global health starts with evidence, impact and readiness. It requires fairness, faster innovation and an alignment of health, sustainability and finance to scale.
- When providers, governments, suppliers and civil society work together progress becomes possible. Here's how it's done.
Well-functioning healthcare systems not only contribute to better population health, they also have an important role to play in reducing inequality and poverty, while promoting social cohesion and social capital.
As global conflict and environmental disasters exacerbate equitable healthcare challenges, the sector is well placed to drive responsible and sustainable practices. Reimagining global health starts with evidence, impact and readiness. It should have fairness at the core, so patients and communities can meet their own health needs sustainably. It also requires faster innovation and alignment of health, sustainability and finance so proven solutions scale for public good.
The private sector cannot tackle these challenges alone. When providers, governments, suppliers and civil society work together – backed by fit-for-purpose regulation and strong advocacy on climate and health – progress becomes possible.
Both representatives of the private medical technology sector must lead the way. It makes sense: embedding responsible and sustainable practices into business strategy is a proven driver of resilience and long-term value creation. Climate pressures intensify inequities. From the natural disasters to conflict-affected regions, there is a clear need and urgency for healthcare solutions designed for global, as well as local, realities.
Collaboration that delivers health and climate impact
The healthcare sector can drive better outcomes with fewer resources through the use of digital, AI-enabled and sustainable solutions that strengthen systems, reduce hospital waste and energy consumption, and expand access to care.
One example of an innovation specifically developed to increase access in low and middle-income countries is Philips’ work on HeartPrint. This venture was designed to provide affordable and efficient cardiovascular diagnostics in India, by empowering people to take care of their own heart health through preventive screening on mobile phones.
When users place a finger on the lens, HeartPrint uses a phone’s camera to measure heart rate, variability, respiratory rate, blood pressure and oxygenation. It creates a cardiac profile to help medical professionals identify health risks and refer patients as needed. Launched in 2024, HeartPrint has reached more than 250,000 people and offers a scalable, global model for improving cardiovascular care and outcomes.
Partnering to close disparities and grow prosperity
To ensure innovation translates into real-world impact, it is important to pair technology with community-focused models that tackle inequality directly. Better health is shaped by medical and non-medical factors, including income, housing and education, as well as the environment. Improving health outcomes gives people the ability to participate meaningfully in society, the local economy and community life.
Equity isn’t an add-on – it’s the operating system. Tools such as Northwell Health’s social vulnerability indices target resources and pair strong primary care and prevention with community support. The result: fewer avoidable hospitalizations, healthier neighbourhoods and people fully engaged in work and their community.
In rural Guyana, Northwell partners with Indigenous communities through community health worker programmes that expand access to essential services while strengthening local workforce capacity. These communities steward some of the most important remaining tropical forests, which serve as critical global carbon sinks. Supporting Indigenous-led health access simultaneously improves outcomes and protects the ecological systems that underpin planetary health, demonstrating the mutually reinforcing nature of climate resilience and equity.
Partnering with national authorities can also be an effective tool for change. Both in Guyana and the Dominican Republic, for example, Northwell works with ministries of health and corporate partners to scale emergency care, nursing workforce development and digital platforms that support both health equity and climate readiness.
Environmental and community prosperity are intertwined. As such, healthcare transformation can help create fairer access, lifting communities socially and economically. When equity leads and technology extends reach, care goes beyond treating disease to strengthening the conditions for health.
Innovation for sustainable care delivery
Improving health outcomes, while driving energy and material efficiency requires end-to-end innovation. It begins early in the product development and ideation phase and continues through logistics, maintenance and responsible reclamation after use.
Digitization and responsible AI are critical too. By using data-driven decision support and remote collaboration, clinicians can avoid unnecessary tests and appointments, streamline patient flow and enable earlier, more precise care. Predictive maintenance keeps equipment running efficiently, cutting downtime and waste.
AI-assisted teleradiology platform Rology is a good example. It instantly connects hospitals and clinics in low and middle-income countries to qualified radiologists and sub-specialists at no setup cost. This tackles a global radiologist shortage and rising imaging demand. When integrated with Philips imaging and digital-health systems, Rology can accept standard image formats and return structured reports directly into local electronic medical records for faster prioritization of urgent cases.
Digital tools can sustain resilient care delivery in complex emergencies and in the context of climate-related instability. Northwell, for example, uses secure telehealth networks to support hospitals in Ukraine. These enable remote care consultations, maintaining continuity of high-acuity services despite disruptions to infrastructure.
All of the partnerships mentioned here support critical healthcare transformation, working towards improved, efficient and effective methods of care, while bringing down operational costs. Partnerships across the healthcare sector contribute to closing the screening and reporting gap, bringing earlier diagnosis and treatment to people who need it.
How the Forum helps leaders strengthen health systems through collaboration
A shared path forward in healthcare sector
If we act now, we can build a future-proof health system that serves people and the planet. Treating healthcare investment as a strategic lever for growth and hardwiring responsible business practices into strategy will help create lasting value and strengthen resilience and prosperity for the long term. Here’s what leaders can do now:
- Invest in what counts: better health, higher productivity, fewer gaps and lower emissions per patient. Scale digital and AI responsibly to deliver more with less, cut waste and improve the patient and clinician experience.
- Build resilient systems: buy energy-efficient, low-resource tech, and design for circularity. Decarbonize operations and supply chains.
- Align policy and partner for scale: set fit-for-purpose standards and incentives that speed up innovation and decarbonization without sacrificing quality or fairness. Use public-private partnerships to turn proven pilots into national programmes.
High performing health systems can drive competitiveness, resilience and prosperity – aligning health, climate and economic priorities for the long term.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Stay up to date:
Global Health
Related topics:
Forum Stories newsletter
Bringing you weekly curated insights and analysis on the global issues that matter.
More on Health and Healthcare SystemsSee all
Ruma Bhargava and Megha Bhargava
March 6, 2026