Asia-Pacific shows how patient engagement is key for healthcare

Patient engagement has a direct impact on national health. Image: Unsplash/CDC

Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:
Health and Healthcare
Listen to the article
- Long-term engagement in healthcare by patients enables deeper preventative care and treatments.
- Patient willingness to interact with healthcare systems often rests on cultural factors.
- The Asia-Pacific region is attempting to overcome a paternalistic model of healthcare to increase patient engagement.
More than a century ago, the delivery of healthcare was based on the simplistic premise of demand and supply depending on a person’s health. People sought care when they fell ill.
Despite advances in modern medicine and a greater understanding of what makes each person unique, this traditional healthcare model still exists. And, as a result, so does a deep-rooted view among most people to seek care only when one needs it. But as the pandemic has shown us, the more informed and engaged people are, the more preventive care and treatments can be optimized. For example, South Korea is regarded as a stand-out in the effective management of COVID-19. The Korea Disease Control and Prevention Agency supported the rapid development of test kits, thereby allowing for efficient testing of COVID-19 across the country and reducing the number of infections and spread of the virus.
As a new white paper, “Asia Pacific’s Patient Engagement Dilemma: The Case for Patient Centricity and Continuous Patient Engagement in Diagnostic Care in Asia Pacific”, reveals, involvement by health systems of patients throughout their healthcare journey and a reciprocal willingness of members of the public to engage with the healthcare ecosystem has a direct impact on national health. This can be seen in the uptake of screening and preventive care, community-based care, health information-seeking behaviours, and home-based monitoring and treatment.
The degree of patient involvement isn’t about being a rich or poor country, rather how people within a particular health system interact with it. Merely being an advanced country does not imply that people are well-informed, enjoy greater engagement with the health system, or get the right care at the right time. If that was the only criteria then the US health system would not have an increasing patient administrative burden, and the National Health Services (NHS) in the UK would not have a waiting period of over 18 weeks.

Why patient engagement matters in Asia-Pacific
While the ability to engage with the healthcare sector is determined by the availability, accessibility, and efficiency of healthcare systems and infrastructure, people’s willingness to engage with them is tied to culture, trust and beliefs.
In most cases, the challenges in healthcare are seen as access issues – a measure of the supply or availability of healthcare resources – and therefore receive the bulk of stakeholder attention. But in fact, simply making resources available cannot solve the dilemma most health systems face today, of growing patient populations, higher costs as well as insufficient resources.
This is where patient engagement becomes critical. Asia-Pacific bears much of the global infectious disease burden, such as tuberculosis, HIV, malaria, hepatitis and diarrhoeal diseases, while witnessing a rise in non-communicable diseases such as cardiovascular diseases, diabetes and various cancers.
Greater patient engagement creates demand for resources or services available within the health system earlier rather than later. Providing them encourages patients to have an interest in, commitment to and reliance on healthcare resources. All of this in turn helps prevent the onset of serious illnesses, increases the quality and length of patients’ lives, lowers the long-term cost of healthcare, and alleviates the associated economic burden in a given society.

Is it in the patient’s interest to be engaged?
Good health as a motivator for people, and the ripple effect it creates, has not been extensively adopted within health system performance indicators. Traditional metrics still rely on singular patient experiences at the point of care instead of their ongoing engagement with the health system.
However, it is worth noting that once people experience the benefits of good health and improved outcomes through ongoing engagement, they will continue to seek ways to maintain this state. This means that, in addition to redoubling efforts to increase access to diagnostic care, stakeholders must act to increase patient engagement and thus the degree to which patients choose to access/continue accessing diagnostic care. Greater patient engagement yields:
● Greater interest in routine screenings for early detection, which in turn leads to a greater likelihood of receiving treatment as early as possible.
● Greater patient compliance with healthcare professionals’ (HCP) advice, recommendations and prescriptions.
● Greater trust in HCPs and health promotion authorities.

No one size fits all
Health systems need to recognize that various factors influence the levels of engagement and the resultant deficit in patient engagement. According to the white paper, some key aspects are:
1. The role of culture in shaping our preference for engagement
The whitepaper found that Asia has a predominantly paternalistic healthcare model, which favours the delivery of diagnoses and treatments over patients’ perceptions of their care. This model of practice focuses on the efficiency of discharging physicians’ duties – and it sits in contrast to “shared decision-making” models we see being practised in some other countries.
To shift away from a paternalistic healthcare model and increase patient engagement, we must encourage deeper relationships between patients and physicians. For example, Singapore is aiming for each household to have their own family doctor from 2023 as part of its national strategy to shift away from traditional illness-based care to patient-centred preventative care.
2. Trust in health authorities
Patients are more engaged when they feel a high degree of comfort with and access to medical professions and health authorities. Factors such as age, sex, religion, education, rural-urban identities and political learnings can impact patients’ trust in the authorities. Public trust is an important aspect for patient engagement, which increases the success of public health interventions such as mass vaccination programmes in controlling the pandemic.
Trust in health authorities is especially critical in combatting healthcare misinformation and supporting effective public health campaigns. Building trust takes time, and it requires a relationship between healthcare authorities (public health institutions, global authorities like the WHO, healthcare professionals, and GPs) and patients. The more health authorities engage and provide effective care, the more opportunities they will have to build trust with patients.
Patient engagement is vital in ensuring that care is delivered appropriately and therefore achieves better healthcare outcomes. To achieve greater patient engagement in Asia-Pacific, all stakeholders have an important part to play in creating a paradigm shift towards a patient-centric model of care.
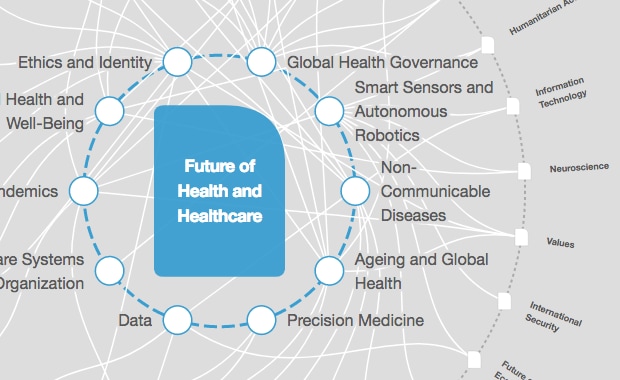
What is the World Economic Forum doing to improve healthcare systems?
Improving healthcare systems hinges on the availability of treatment options, access to preventative measures such as diagnostics and screenings, and patient engagement. While the industry focuses on increasing the availability and access to effective and efficient diagnostics and treatment options, the push for patient-centric health has never been so crucial. It is only when patients are fully engaged that we can develop effective health promotion strategies to prevent serious illness, increase the quality and length of patients’ lives, and lower the long-term costs of healthcare.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The Agenda Weekly
A weekly update of the most important issues driving the global agenda
You can unsubscribe at any time using the link in our emails. For more details, review our privacy policy.
More on Health and HealthcareSee all
Johnny Wood
April 17, 2024
Adrian Gore
April 15, 2024
Carel du Marchie Sarvaas
April 11, 2024
Nancy Ip
April 10, 2024
Shyam Bishen
April 10, 2024